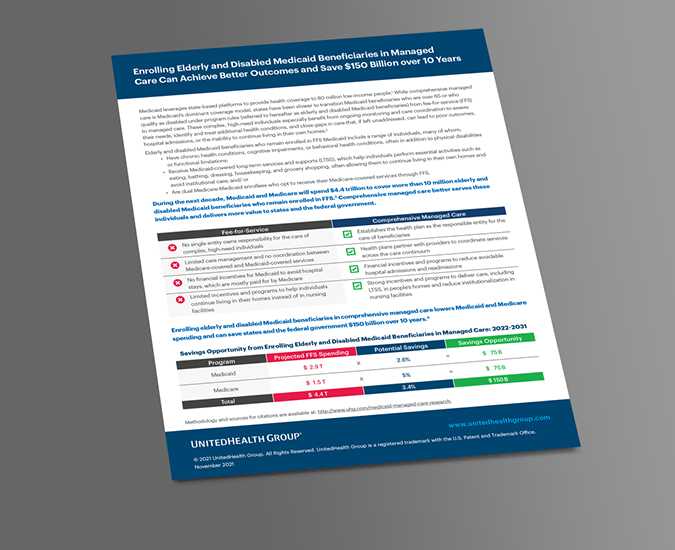
Medicaid beneficiaries who are elderly or living with disabilities benefit from ongoing monitoring and care coordination.
However, states have been slow to transition these complex, high-need individuals from fee-for-service to managed care.
The Numbers That Matter

Managed Care Can Also Help:
Coordinate care for individuals.
Coordinate care for individuals.
Reduce avoidable hospital admissions and readmissions.
Reduce avoidable hospital admissions and readmissions.
Provide individuals with long-term support services.
Provide individuals with long-term support services.
Lower Medicaid and Medicare spending.
Lower Medicaid and Medicare spending.
What We're Doing
![]()
7.5 million people served by Medicaid programs in 31 states and the District of Columbia, including:
![]()
375,000 individuals in 22 states who are age 65 or older or living with disabilities.
![]()
1.2 million people in Dual Special Needs Plans in 37 states and the District of Columbia.

Share This Story