With a global pandemic continuing to interrupt people’s everyday lives, access to behavioral health and emotional support has never been more critical. Optum continues to respond to the need by significantly expanding the availability of telehealth visits, including growing the number of providers available to see patients virtually.
Early data suggests that providers and members are benefiting from a transition from in-person visits to telehealth sessions delivered through telephone and video chat platforms, or through Optum’s proprietary behavioral health virtual visit platform. By the end of March, 33% of all care was shifted to telehealth with the following results:
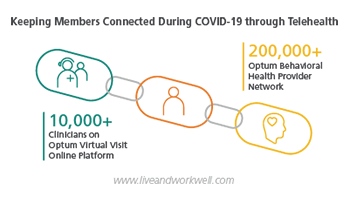 Behavioral health providers and members have new ways to deliver or seek care. The more than 200,000 Optum behavioral health providers are now able to deliver care through alternative technologies like telephone visits or video chat services. This policy applies to commercial, Medicare and Medicaid members served by Optum, and keeps members connected to applied behavior analysis clinicians, group therapy and intensive outpatient program sessions. Optum recently extended this flexibility through at least May 31, 2020.
Behavioral health providers and members have new ways to deliver or seek care. The more than 200,000 Optum behavioral health providers are now able to deliver care through alternative technologies like telephone visits or video chat services. This policy applies to commercial, Medicare and Medicaid members served by Optum, and keeps members connected to applied behavior analysis clinicians, group therapy and intensive outpatient program sessions. Optum recently extended this flexibility through at least May 31, 2020.
- Provider participation and member utilization of Optum’s proprietary behavioral health virtual visit platform are growing. In March, Optum began to recruit new providers and accelerate approvals of providers interested in offering virtual care through its online platform. Since then, the number of providers participating in this network has increased by more than 45%, bringing the number of certified virtual visit providers to more than 10,000, and the numbers continue to grow. In addition, the number of appointments scheduled by members through Optum’s virtual visit platform is 52% higher than pre-COVID-19 averages.
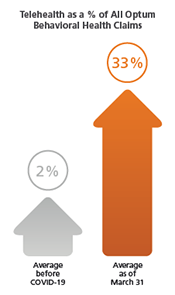 Early claims data indicates a significant shift in the use of telehealth for behavioral health care. Normally, about 2% of all behavioral health claims Optum receives are for a telehealth visit. By the end of March, approximately 33% of all behavioral health claims for Optum members were for a telehealth visit. The most recent claims data indicates that the proportion of telehealth visits continues to sharply increase.
Early claims data indicates a significant shift in the use of telehealth for behavioral health care. Normally, about 2% of all behavioral health claims Optum receives are for a telehealth visit. By the end of March, approximately 33% of all behavioral health claims for Optum members were for a telehealth visit. The most recent claims data indicates that the proportion of telehealth visits continues to sharply increase.
“We will continue to ensure the people we serve are able to stay connected with behavioral health care providers during COVID-19,” said Rebecca Schechter, CEO, Optum Behavioral Health. “We’re also doing more by proactively reaching out to our most vulnerable members so they understand how to best continue their treatment, including prescription refills.”
Additional Optum efforts to serve people needing behavioral and emotional support include:
- Genoa Healthcare, an Optum business that runs pharmacies within community behavioral health clinics, has enabled 14 community mental health clinics to use its telepsychiatry platform to remotely treat their patients. Genoa Pharmacy has shifted to home and curbside delivery of medications and Genoa's telepsychiatry is connecting patients with physicians in their homes to help hundreds access needed psychiatric care. These efforts are helping ensure Genoa’s 1 million patients, many of whom are diagnosed with severe mental illness and substance use disorders, continue to receive treatment.
- Sanvello Health, a UnitedHealth Group company, has made their premium services free to anyone, and its clinician dashboard free to professionals during the national crisis. Sanvello is now ranked the No. 1 app for people looking to manage stress and anxiety. By the end of March, weekly registrations for Sanvello were 200% higher than prior averages.
- Optum’s Employee Assistance Program (EAP), serving more than 15 million members globally, is providing members resources they need online or over the phone. Optum EAP is seeing increased demand from members seeking emotional, financial and work-life support, typically four to eight weeks from the peak impact in any region. The most frequent requests for assistance from members include addressing opportunities to better manage stress and anxiety, addressing relationship issues, identifying child or elder care, and accessing home-schooling resources.
- The free Optum Emotional Support Help Line (866-342-6892) continues to support people with tips on self-care and connections to local resources.
Optum behavioral health and EAP members can find more information by logging on to their Live and Work Well account at http://www.liveandworkwell.com.
For providers, more information can be found on Provider Express at www.providerexpress.com.
Share This Story